Cancer treatment in Spain is undergoing a profound transformation, thanks to remarkable advances in genomic medicine. This cutting-edge field is paving the way for personalized therapies that target specific genetic alterations in tumors, offering new hope to patients across the country.
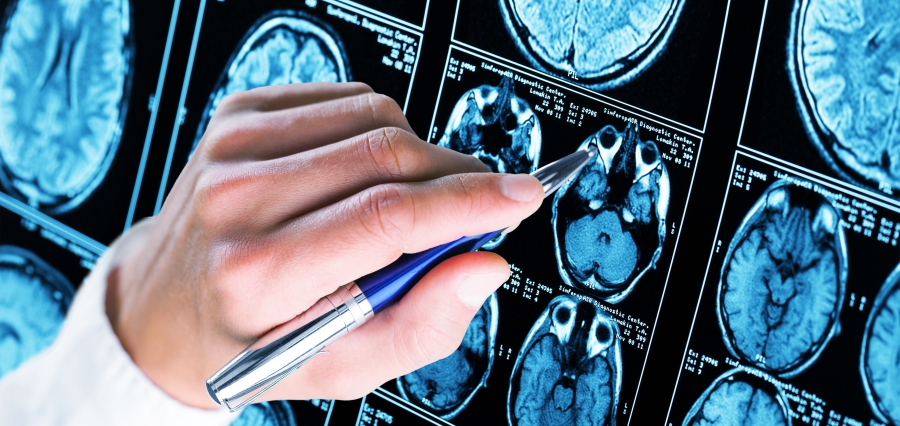
At the forefront of this revolution is the treatment of non-small cell lung cancer (NSCLC), where genomic profiling has led to the development of numerous targeted therapies. The European Commission has given the green light to over 20 such treatments, each designed to address specific genomic alterations involving genes like ALK, RET, ROS1, EGFR, BRAF, NTRK, KRAS, and MET.
However, the promise of these innovative treatments has been tempered by the challenges of implementation within the Spanish healthcare system. A comprehensive review conducted by the Spanish Lung Cancer Group (SLCG) revealed a significant gap between approval and accessibility. Of the many driver alterations that can now be targeted, only five are currently covered for therapeutic purposes by Spain’s National Health System (NHS).
This disparity in access to cutting-edge cancer treatments is not unique to Spain but reflects a broader issue across European countries. The SLCG has emphasized the urgent need to bridge this gap, calling for improved access to targeted therapies to ensure that Spanish patients receive the most effective, personalized treatments available.
The potential of genomic medicine extends beyond lung cancer. In the realm of soft tissue sarcomas (STS), next-generation sequencing (NGS) is emerging as a powerful tool to guide treatment decisions. Despite the typically low mutational burden and scarcity of recurrent targetable alterations in most STS histotypes, retrospective studies have identified various gene mutations, fusions, and amplifications that could inform treatment strategies.
Anecdotal evidence suggests that targeted therapies, whether administered off-label or through clinical trials, have shown promise in various STS histotypes. However, access to these therapies remains inconsistent, with significant disparities in the availability of NGS platforms and molecularly driven treatments across different regions and countries.
The transition from hype to hope in genomics-guided therapies is evident in initiatives like the Cancer Genomics Initiative in Maine, USA. This program successfully provided access to genomic tumor testing (GTT), clinician educational resources, and genomic tumor boards in community practices. The initiative demonstrated that with proper dissemination and supportive infrastructure, GTT can benefit cancer patients even in rural community oncology settings.
In Spain, the SLCG’s review underscores the need for similar initiatives to improve access to targeted therapies. By expanding access to genomic profiling and supporting clinical decision-making, Spain can ensure that more patients benefit from personalized, targeted treatments.
The future of genomic medicine holds even greater promise. Researchers are developing therapies to target previously “undruggable” alterations, such as the selective inhibitor PC14586 for the TP53 Y220C mutation. As our understanding of molecular genetics continues to evolve, new targets are being identified, and efforts are underway to unlock the full potential of these therapies.
To fully harness the benefits of genomic medicine, advances in organ targeting are crucial. Emerging technologies aim to improve the delivery of genomic medicines, potentially expanding their efficacy and applicability across various cancer types.
The impact of genomic medicine extends beyond individual patient outcomes. By enabling more precise and effective treatments, these advances have the potential to reduce healthcare costs associated with ineffective therapies and managing treatment side effects. Moreover, the data gathered from genomic profiling contributes to a growing body of knowledge that can inform future research and drug development.
However, the integration of genomic medicine into standard clinical practice faces several challenges. These include the need for standardized testing protocols, interpretation of complex genomic data, and education of healthcare providers on the latest advances in the field. Additionally, ethical considerations surrounding genetic information and data privacy must be carefully addressed.
To overcome these hurdles, a multifaceted approach is needed. This includes:
- Increased funding for genomic research and implementation of genomic testing in clinical settings.
- Development of clear guidelines for the use of genomic information in treatment decision-making.
- Enhanced education and training programs for healthcare professionals in genomic medicine.
- Improved collaboration between researchers, clinicians, and pharmaceutical companies to accelerate the development and approval of targeted therapies.
- Advocacy for policies that ensure equitable access to genomic testing and targeted therapies across all regions of Spain.
As Spain continues to navigate the evolving landscape of genomic medicine, it is crucial to strike a balance between innovation and accessibility. By addressing the current disparities in access to targeted therapies and investing in the infrastructure necessary to support genomic medicine, Spain can position itself at the forefront of personalized cancer care.
The promise of genomic medicine in oncology is clear: more effective treatments, improved patient outcomes, and a deeper understanding of cancer biology. As we look to the future, the continued advancement and integration of genomic medicine into Spanish healthcare holds the potential to transform the lives of countless cancer patients, offering hope where once there was little.